A new wave of COVID-19 is bearing down on the city, with health experts unsure about what impact it will have; Mayor Eric Adams tested positive Sunday, and is working remotely, according to City Hall.
Many residents are now also facing another new uncertainty: the cost of COVID-related care.
Last month, a federal government fund that reimbursed pharmacies, hospitals and other health care providers for the costs of COVID-related care ran dry, without being refilled by Congress.
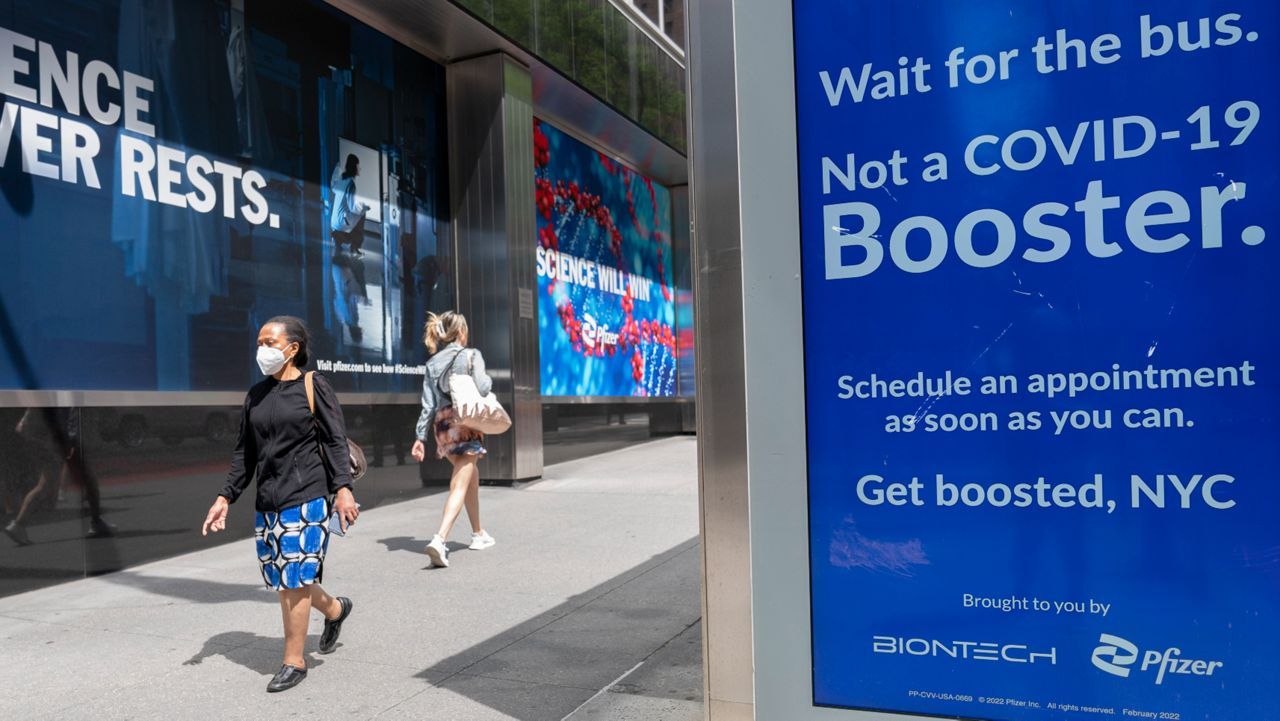
Since then, many private health providers, no longer able to receive money from the government to cover COVID-19 costs for uninsured people, or costs that may have covered copay fees, have begun charging for such care. Testing at city-run sites remains free.
Reports have begun to fill social media of people being surprised by quotes or charges for PCR tests that have been free for much of the pandemic.
The wave of costs, coming as the omicron subvariant BA.2 is causing a slow rise in infections in the city, has health experts and doctors concerned. Making tests prohibitively expensive, especially for uninsured or underinsured people, they say, will only exacerbate existing health care disparities, and make people less likely overall to seek medical care.
It’s not clear, either, that Congress will provide enough funding to restore the reimbursement program at all, leaving uninsured Americans to pay for testing and treatment at private providers indefinitely.
“It does long-range damage every time someone shows up to get care and gets surprised by a giant bill,” said Dr. Stephanie Woolhandler, a professor of urban public health at Hunter College. “It’s damage for COVID, it’s damage for when the next pandemic comes around, it’s damage when someone has a heart attack.”
Here’s what you need to know about costs of COVID-related care in New York City.
Can a health care provider charge for a COVID-19 vaccine?
No, according to Jennifer Tolbert, director of state health reform at the Kaiser Family Foundation.
Any health care provider or government that agreed to distribute vaccinations has to adhere to federal rules that prohibit charging anyone, with any insurance background, for the shot.
The federal government has already covered the costs of buying the vaccines, as well as shipping them to states, cities and health care providers. The remaining costs associated with administering the vaccines can be billed to either government insurance or private insurance, Tolbert said.
“No entity can charge anyone for the cost of the vaccine, because it’s already been paid for,” Tolbert said.
Does New York City still offer free testing, vaccination and treatment for COVID-19?
PCR testing for COVID-19 is free at all city-run providers, including the NYC Health and Hospitals Network and Gotham Health clinics. For a list of locations and hours, including regular rapid test pick-up locations, click here.
If you test positive for COVID-19 and experience symptoms, you may be eligible for free treatment, provided and delivered by the city. (Mayor Adams is currently taking free antiviral pills provided by the city, according to his representatives.) The call line to sign up for the treatment is open from 9 a.m. to 9 p.m., seven days a week, at 212-COVID19.
The city government is planning to distribute 6.33 million at-home rapid tests during April at pick-up locations around the city and through 2,500 partner organizations, according to Adam Shrier, a spokesperson for the city’s Test and Trace initiative. These tests are separate from the city’s ongoing testing in schools, Shrier said, which administers PCR tests each week to at least 10% of students who have opted into the testing program.
To see a list of pick-up locations, visit this website.
Community-based organizations can join a wait list to distribute at-home tests here.
There are two tests in each rapid test kit. Should I use both each time I test?
Health experts say that taking two tests increases the likelihood of an accurate result.
Studies have suggested that false positives, receiving a test result indicating you have COVID-19 when you do not, are rare, meaning that when you test positive on a rapid test, you are highly likely to actually have COVID-19. False negatives (a test result indicating you do not have COVID-19 when you do) are more common. Two negative tests, medical experts say, means it is very unlikely you have COVID-19, while at least one positive test suggests you are likely infected.
If I have Medicaid or Medicare, can I be charged for COVID-related treatments?
If you are on Medicaid, you should be able to get tested, treated and vaccinated for COVID-19 for free, Tolbert said.
“People on medicaid should not face any costs for these services,” Tolbert said.
People on Medicare, the government insurance for people aged 65 and up, should not face costs for COVID testing, but may face cost sharing, such as copays, for COVID treatment, such as when they are admitted to a hospital or visit a doctor, she said.
Can I get rapid tests with insurance?
If you haven’t already, you can get up to two sets of at-home COVID-19 tests (meaning four tests total) through the federal government, by ordering from this site.
Private insurers are required to cover up to eight rapid tests per member per month. This policy does not apply to people with Medicaid or Medicare Advantage, according to the Kaiser Family Foundation. Insurers, however, are allowed to cap reimbursement for tests at $12 per test; some pharmacies are selling tests for double that amount or more.
If you have an HSA or FSA spending account: According to the Internal Revenue Service, rapid tests (as well as masks and some other protective equipment) are eligible for reimbursement through such programs. Call your particular program to confirm the reimbursement process.
Which private providers are charging for tests, and which aren’t?
Since the federal money stopped flowing, there is a mix of private providers and pharmacies that are still offering free COVID-19 services, and those that are not.
CityMD, a popular chain of urgent care clinics, is charging for COVID-19 tests and treatments, according to its website. For people with insurance, visiting a CityMD location for COVID-related care may result in a copay or deductible payment. On social media, some people have reported being quoted or charged hundreds of dollars for COVID-19 tests at City MD locations. A representative for CityMD did not respond to a request for comment.
SOMOS Community Care, a network of providers with clinics in every borough but Staten Island, serves many immigrant patients, and has continued to provide COVID-19 tests and vaccination without charging. (It does not provide treatment for COVID-19.) SOMOS has a contract with New York City and the state to be paid for providing free COVID-19 care, according to a spokesperson for the company.
Walgreens, which owns the Duane Reade pharmacy brand, and CVS are not charging patients for COVID-19 testing, according to representatives for the companies. Walgreens also provides COVID-19 treatments at no cost.
Rite Aid said it was offering free testing through May, through a contract with the city’s Department of Health and Human Services. People covered by Medicare Part B can also receive up to eight at-home rapid tests per month at RiteAid stores.
Why isn’t the federal government covering these costs anymore?
During negotiations over the federal budget last month, congressional leaders hit an impasse over a large tranche of money requested by the White House to continue funding several COVID-related programs. Congress eventually passed the budget without the COVID-19 resources, leaving a crucial program, the COVID-19 Uninsured Program, unfunded.
On March 22, the program stopped accepting reimbursement requests from health care providers for COVID-19 tests, and for vaccinations on April 5. Without the money, the White House says, it cannot purchase additional tests, treatments or even more vaccines when current supplies run out.
Senate leaders announced last week that they reached a deal on COVID-19 funding, at a much smaller amount than originally requested by the White House — $10 billion out of a hoped-for $22.5 billion. But this week, Senate Republicans blocked debate on the bill, seeking to get Democratic leaders to vote on an amendment that would preserve a ceiling on immigrants allowed into the country put in place under former President Donald Trump.
The Senate is in spring recess and won’t be able to take up the bill until the end of the month.
Will Congress refill the reimbursement fund?
Health experts are still hopeful that the funding will be restored, but they say that the uncertainty created since it lapsed has damaged public health goals, especially in communities of undocumented people where insurance coverage is low.
“It’s critical that we get this funding back in place,” Woolhandler said.
But Tolbert said it is not clear that the federal government will get enough money from Congress to replenish the reimbursement fund.
Talking points released on the Senate’s $10 billion compromise do not require that any of the money go to the reimbursement fund, she said. The fund, created by the Trump administration early on in the pandemic, is not codified in law. It has already spent more than $19 billion to reimburse providers on testing, treatment and administering vaccines for uninsured people.
The Senate’s agreement, however, does require that $5 billion be spent on treatments for COVID-19, leaving $5 billion for both vaccine and testing costs, including reimbursing the uninsured fund.
With the FDA considering approving a second booster dose for all adults, the federal government may have to spend a substantial chunk of that $5 billion on more vaccines — and spending on vaccination administration for the uninsured may win out over reimbursing for testing and treatment for that group.
“At the end of the day, that’s just not a lot of money if you want to ensure that vaccines remain available for all who may need them,” Tolbert said.
Right now, with case counts relatively low nationally, Tolbert said, testing in general is not as vital.
But that can always change, and without a major influx of funding from Congress, uninsured people will face major cost barriers to testing and treatment.
“The bigger issue, and the thing to think about, is what happens if there is another surge?” she said.