Though the pandemic is securely in the rearview mirror, the demand for mental health providers and services continues to rise, as does the need for more innovative solutions.
In the first part of our Exploring Your Health series on post-traumatic stress disorder, National Health Reporter Erin Billups takes a look at the effort underway to treat the common mental health condition. Notice to viewers: this piece includes references to sexual assault.
What You Need To Know
For Claire Dowdle Cina, fear became a constant companion.
“Something would trigger me and my body would be just on fire with anxiety-like panic,” said Cina.
A psychotherapist herself, Cina knew the root cause; starting when she was just three years old, she suffered sexual abuse at the hands of a family member for nearly a decade.
Through her childhood she would immerse herself in reading and sports to cope, but as she entered adulthood her symptoms changed.
“I started just having a lot of intrusive thoughts and emotional flashbacks. And it was just all related to either current romantic partners or different sexual things that were coming across a screen,” said Cina. “It became more haunting, I guess, and a lot of nightmares.”
Cina was experiencing post-traumatic stress disorder, or PTSD. The disorder is often associated with veterans but can affect anyone who has experienced a traumatic event.
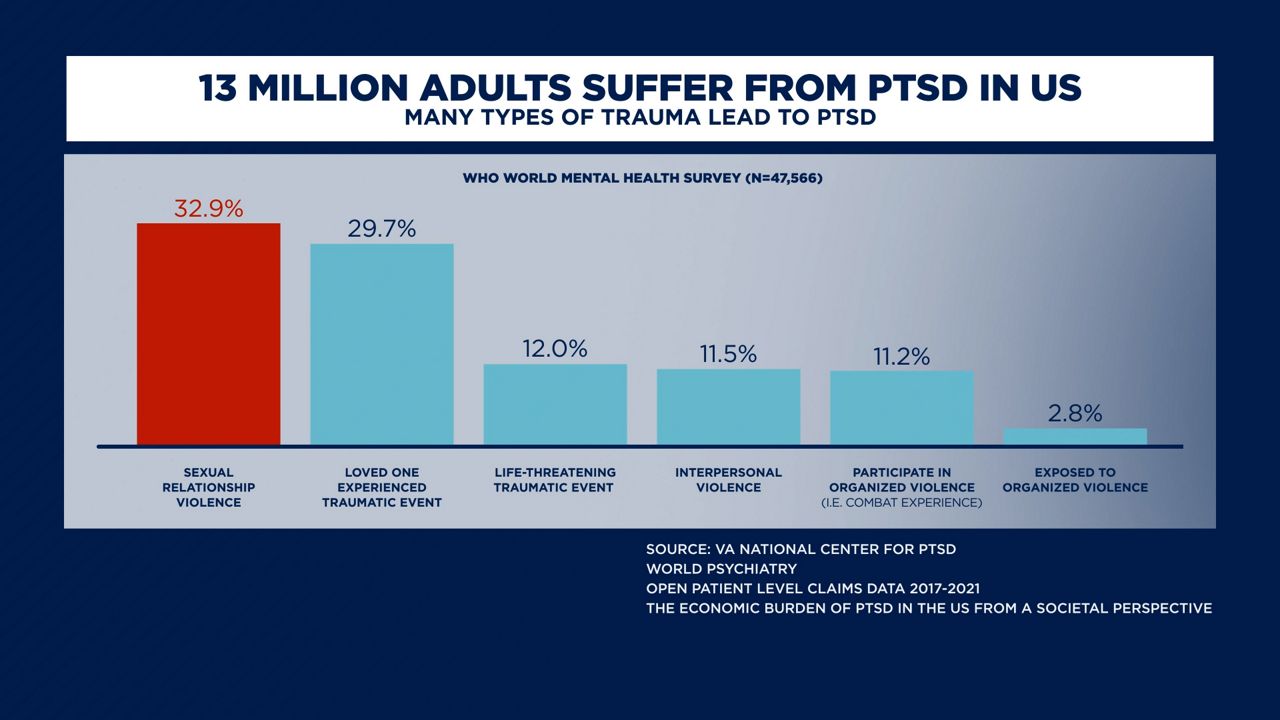
13 million adults suffer from PTSD in the U.S –with over 30% of sufferers being survivors of sexual relationship violence, like sexual assault or beating. The condition can cause intense emotional and physical reactions for months or years after a traumatic event.
“I was aware at that point that what was happening was not about really what was going on in the present moment,” said Cina.
She tried different approaches to facing her trauma, like talk therapy, antidepressants and the hallucinogenic drug ayahuasca. Cina credits each with helping her heal, but felt she needed something more impactful as she moved toward the next chapter of her life.
“I really wanted to be a mother, and I was worried that I was going to have a hard time going through pregnancy and having a lot of invasive experiences around my body,” Cina said.
Cina was following developing research and enrolled as a participant in a phase three trial sponsored by MAPS Public Benefit Corporation, a research and psychedelic drug development organization.
The study combined MDMA–the active ingredient in the party drug Ecstasy – with talk therapy to treat PTSD.
“It gives a new approach to a very specific experience that I don't think any other mental health treatment can access,” said Cina.
In addition to three 8-hour MDMA-assisted therapy sessions, trial participants meet with therapists throughout the course of the three-month experience.
Dr. Jennifer Mitchell, is a neurology professor at the University of California, San Francisco, and is a lead author of the study. She says the goal is to see if the MDMA- assisted therapy can go beyond easing symptoms, to erasing them altogether.
“We do take special care to really craft an environment that's going to make a participant feel very well contained, very well held, very well supported,” said Mitchell.
The 2021 data found the treatment worked for a majority of trial participants, all of whom had been diagnosed with PTSD for an average of 14 years prior.
“We saw 88% of the people had a clinically significant improvement in their PTSD,” said Amy Emerson, CEO of the MAPS Public Benefit Corporation.
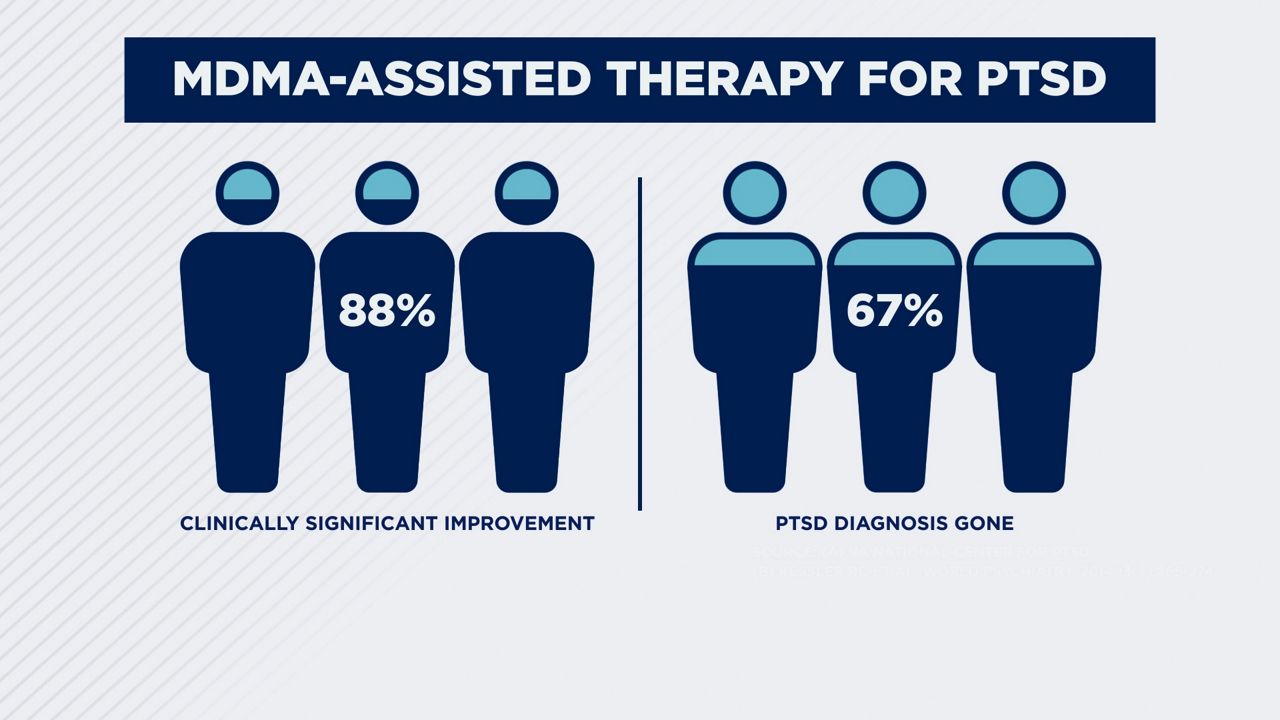
New 2023 data found more than 71% of participants no longer met the criteria for a PTSD diagnosis.
Emerson has been involved in research into MDMA for two decades and says their data also shows that the treatment sticks.
“We saw that it was durable. People maintained that improvement in their symptoms,” said Emerson. The latest data, she says, confirms previous trial findings. “We did see once again, the decrease in their symptoms, loss of diagnosis and this again, ability to have a better quality of life.”
These scientists say MDMA helps people feel safe to open up in a way that allows deep work to occur. “There's these subjective effects of it that decrease fear, increase trust, increase somebody's ability to talk about the trauma without re-traumatizing themselves,” said Emerson.
It’s theorized that the treatment may help break the cycle of trauma in the brain. In a person experiencing PTSD, the amygdala, which senses threats, confuses memories of past traumatic events with an imminent threat. This happens when a trigger, such as a smell or sound, reminds a survivor of their traumatic experience.
A common example of this is when combat veterans react negatively to the sound of fireworks. The amygdala responds as though you are experiencing the trauma in that moment and sends signals to the body to escape it.
“MDMA helps you sort of retrieve and reprocess deeply emotional memories. And so the hope is that sort of this reprocessing allows them to sort of be released,” said Mitchell.
Mitchell says MDMA and other psychedelics help create a window of opportunity or flexibility to correct wrongs baked in from the past.
“They seem to reopen this critical period for social and emotional learning, which gives you this window of opportunity, to sort of correct some wrongs that have been with you into adulthood,” said Mitchell.

Dr. Rachel Yehuda is a professor of psychiatry & neuroscience of trauma at the Mount Sinai Icahn School of Medicine. She said there’s still so much to learn about what MDMA does to the body and brain.
“There are a lot of theories about neuroplasticity and how psychedelics in general may allow you to metaphorically build new railroad tracks,” said Yehuda. “People tend to look at imaging studies and get very excited about different brain regions starting to talk to each other. What that reflects is the fact that people that are taking psychedelics are having a very powerful inner experience. But what it all means, we don't really know yet. But these signals are exciting.”
Yehuda is studying MDMA-assisted therapy as a treatment for PTSD in veterans. She said more research is needed to understand why this treatment works for some and not others.
Yehuda stresses that patients who have success with MDMA- assisted therapy tend to have one thing in common--a willingness to, with the drug’s help, do the hard emotional work required during treatment sessions.
“I like to use the metaphor of an e-bike. Sometimes when you're going up a very steep hill,” said Yehuda. “If you have a little motor on your bike, you still have to pedal very, very hard, but you can get up that hill.”
Cina agrees. Healing takes work, even with the help of the MDMA. “It's not just that you are just sitting there, you take this drug and then poof, right? It's processing, it's working,” said Cina. “I really felt like I had to be willing to be with it and go there and try something different.”
Cina’s hard work paid off. “I was able to really experience the emotions that I had had in the past that I hadn't been able to really access before. So it felt almost like purging some of that.”
The MDMA-assisted therapy also shifted how she viewed her traumatic childhood experiences.
“It helped me to understand the grief associated with what had happened, the sort of terror or disgust or some of the other things that I was struggling so much with,” said Cina. “And have a lot more compassion for myself as a child.”

Cina says because of the treatment she found strength to face her fear of pregnancy. “I was able to go through that experience, yes, with some anxiety, but in a much more calm and joyful way and to have two amazing birth experiences.”
She hopes now to use her experience to help other people dealing with PTSD. Her blog seeks to offer advice and community to those who are stil working through their trauma.
Three years after completing treatment, Cina is still able to sit with her emotions in a new way. “My ability to be present is helping me actually have this hope for my life in a different way, of just being with my kids and feeling really in the moment,” said Cina. “I think that's shifted a lot in just being more bright about things.”






