Hawaii has entered a settlement between the 50 states and Walgreens stemming from allegations that the retail pharmacy chain unlawfully billed government health care programs for prescriptions that were never collected or otherwise received by patients.
The overall $97.8 million settlement resolves a pair of qui tam lawsuits (suits filed by a private individual on behalf of the government) that accused the Deerfield, Illinois-based company of unlawfully billing Medicare, Medicaid and other government health care programs for prescription drugs that were never picked up by the beneficiaries. The charges, totaling tens of millions of dollars, were billed between 2009 and 2020.
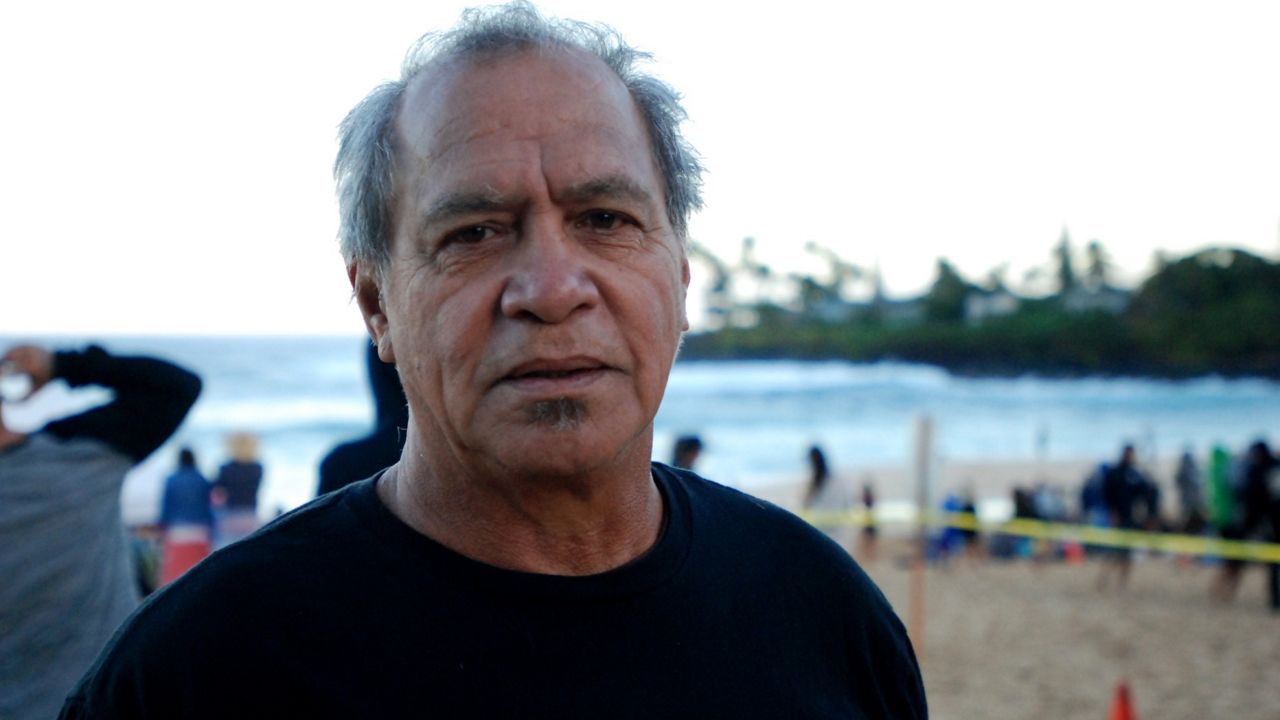
“This is a significant win in the fight against health care fraud in our country,” said Landon Murata, director of the Medicaid Fraud control Unit in Hawaii. “We appreciate all the hard work and dedication of our federal and state partners who made this settlement possible. It is important that remain vigilant to ensure that taxpayer dollars dedicated to supporting our critical healthcare programs like Medicaid, are not being squandered.”
Walgreens has since updated its billing systems to prevent future unlawful billings for uncollected prescriptions. The company was credited for self-disclosing certain claims and refunding more than $66 million with the settled claims.
The total recovery for all Medicaid programs under the settlement is $9.6 million. Of that amount, Hawaii will receive $3,524.83 in recoveries.
A National Association of Medicaid Fraud Control Units team investigated the allegations in conjunction with the U.S. Department of Justice and United States Attorneys’ Offices in Texas and Florida. The NAMFCU Team included representatives from the respective Office of the Attorney General for the states of Wisconsin, California, Texas, Maine, Oregon and Massachusetts.
Entering into the settlement agreement on behalf of the state was Murata for the Department of the Attorney General and Judy Mohr Peterson. Med-QUEST Division administrator at the Department of Human Services.
Michael Tsai covers local and state politics for Spectrum News Hawaii. He can be reached at michael.tsai@charter.com.