Alarmed by yet another jump in syphilis cases in newborns, U.S. health officials are calling for stepped-up prevention measures, including encouraging millions of women of childbearing age and their partners to get tested for the sexually transmitted disease.
What You Need To Know
- Syphilis cases in U.S. newborns again are on the rise
- It has health officials calling for new measures to stop the increase, including encouraging millions of sexually active women of childbearing age and their partners to get tested
- The Centers for Disease Control and Prevention says more than 3,700 babies were born with congenital syphilis in 2022
- That's 10 times more than a decade ago and a 32% increase from 2021
More than 3,700 babies were born with congenital syphilis in 2022 — 10 times more than a decade ago and a 32% increase from 2021, the Centers for Disease Control and Prevention said Tuesday. Syphilis caused 282 stillbirth and infant deaths, nearly 16 times more than the 2012 deaths.
The 2022 count was the most in more than 30 years, CDC officials said, and in more than half of the congenital syphilis cases, the mothers tested positive during pregnancy but did not get properly treated.
The rise in congenital syphilis comes despite repeated warnings by public health agencies and it's tied to the surge in primary and secondary cases of syphilis in adults, CDC officials said. It's also been increasingly difficult for medical providers to get benzathine penicillin injections — the main medical weapon against congenital syphilis — because of supply shortages.
"It is clear that something is not working here, that something has to change," the CDC's Dr. Laura Bachmann said. "That's why we're calling for exceptional measures to address this heartbreaking epidemic"
The federal agency wants medical providers to start syphilis treatment when a pregnant woman first tests positive, rather than waiting for confirmatory testing, and to expand access to transportation so the women can get treatment. The CDC also called for rapid tests to be made available beyond doctors' offices and STD clinics to places like emergency rooms, needle-exchange programs and prisons and jails.
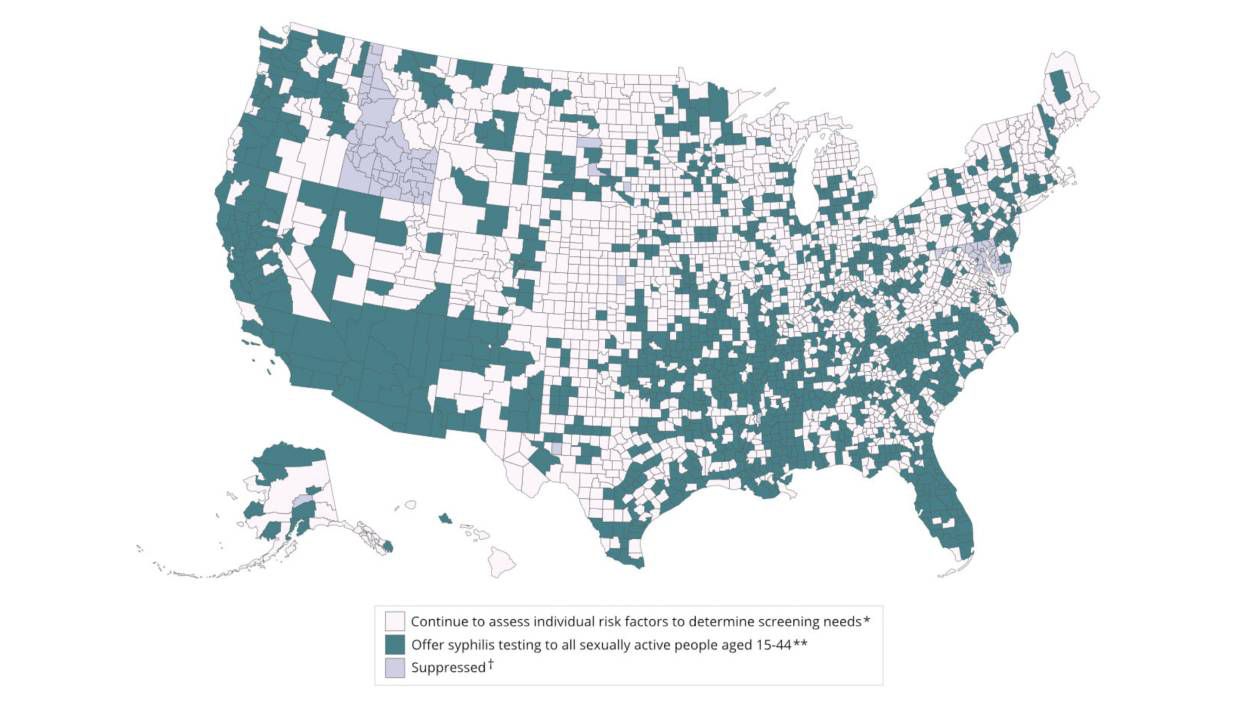
Federal officials again advised sexually active women of childbearing age and their partners to get tested for syphilis test at least once if they live in a county with high rates. According to a new CDC map and definition, 70% of U.S. adults live in a county with high rates. That's likely tens of millions of people, according to an Associated Press estimate based on federal data.
The CDC's recommendations are just that; there is no new federal money going out to state and local health departments to bolster testing or access. Some state health departments have already said they're stretched thin when it comes to treatment and prevention, though Illinois announced last week it was starting a phone line for health care providers to help with record searching, consultation and assistance with mandatory reporting.
Syphilis is a bacterial infection that for centuries was a common but feared sexually transmitted disease. New infections plummeted in the U.S. starting in the 1940s when antibiotics became widely available and fell to their lowest mark in the late 1990s. By 2002, cases began rising again, with men who have sex with other men being disproportionately affected, though the STD is spreading among several demographics.
In congenital syphilis, moms pass the disease on to their babies, potentially leading to death of the child or health problems for the child like deafness, blindness, and malformed bones. Case rates have been rising across racial and ethnic groups.
Dr. Mike Saag, an infectious diseases expert at the University of Alabama at Birmingham, said syphilis can be "a silent infection" in women because it's tricky to diagnose without a blood test — not everyone gets painless sores, wart-like lesions or other visible symptoms.
The CDC has long recommended that all pregnant women should be tested for syphilis at their first prenatal visit, but poor access to prenatal care — largely in rural areas of the U.S. — can make that difficult. Nearly 40% of last year's congenital syphilis cases involved mothers who didn't have prenatal care, the CDC said.
If syphilis is diagnosed early in a pregnancy, the threat of passing it to the baby can be removed by a single penicillin shot. But experts say the later you get into pregnancy, the more likely you'll need multiple shots, and they have to be completed at least 30 days before delivery.
"I have had patients who have been on (a three-shot) regimen who then miss a shot," said Dr. Nina Ragunanthan, an OB/GYN at the Delta Health Center in Mound Bayou, Mississippi. "So they are trying to get their shots, but if they don't get the three in a row, because of transportation issues, because of job issues, child care issues, any number of reasons that prevent them from coming back, they don't complete their treatment."
Plus, the shortage of shots makes the task of getting syphilis numbers down difficult, health officials across the U.S. told the AP. Patients who are not pregnant can use the antibiotic doxycycline to treat syphilis, but health officials are concerned that the 14- to 28-day timeline of treatment is difficult to complete, leaving infected people uncured.
Pfizer is the nation's sole supplier of the penicillin shot. Earlier this year, company officials said it was in short supply because of increased demand. Pfizer also said the shortage may not be resolved until next year.
The CDC said the shortage didn't affect the 2022 congenital syphilis case numbers and that, despite the shortage, it isn't aware of patients not getting their needed shots.